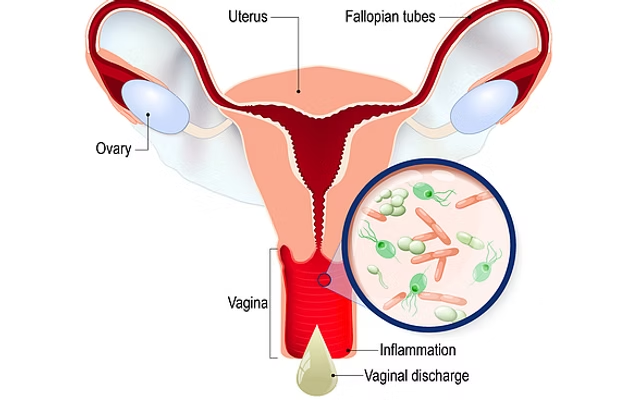
Vaginal candidiasis, often referred to as a yeast infection, is a condition caused by the overgrowth of Candida albicans, a type of fungus naturally present in the body. While it is commonly found in areas like the mouth, digestive tract, and genital region, certain conditions can disrupt the balance, allowing the fungus to multiply and cause an infection. This issue is widespread among women but can also affect men and other parts of the body in different forms.
What Is Vaginal Candidiasis?
Vaginal candidiasis occurs when the natural environment of the vagina is disrupted, leading to an excessive growth of Candida. Normally, the body’s immune system and the beneficial bacteria in the vaginal microbiota help keep Candida in check. However, when these defenses are compromised, the fungus can thrive, resulting in uncomfortable symptoms.
Recognizing the Symptoms
The symptoms of vaginal candidiasis can vary from mild to severe, but some of the most noticeable include:
- Persistent itching and irritation in the vaginal area.
- Redness and swelling of the vulva.
- Thick, lumpy discharge that resembles cottage cheese, usually odorless.
- Burning sensations during urination or after intercourse.
- Tiny fissures or cracks on the vulvar skin caused by excessive scratching.
- In more severe cases, the inflammation may spread, causing significant discomfort.
It’s important to note that symptoms can overlap with other conditions, such as bacterial vaginosis or sexually transmitted infections, so a proper diagnosis is essential.
What Causes Vaginal Candidiasis?
Understanding the triggers behind this condition can help prevent recurrent infections. Key factors that contribute to Candida overgrowth include:
- Antibiotics: Overuse or inappropriate use of antibiotics can deplete beneficial bacteria, disrupting the vaginal microbiota and allowing Candida to flourish.
- Hormonal fluctuations: Pregnancy, menopause, and even hormonal contraceptives can affect the vaginal environment, increasing susceptibility.
- Diabetes: High blood sugar levels provide an ideal environment for fungal growth, particularly in uncontrolled diabetes.
- Weakened immune system: Conditions like HIV, chronic illnesses, or treatments such as chemotherapy reduce the body’s ability to control Candida.
- Improper hygiene: Excessive washing, use of harsh soaps, or frequent vaginal douching can disturb the natural pH and microbiota balance.
- Clothing choices: Wearing tight, non-breathable fabrics traps heat and moisture, creating a favorable environment for fungal growth.
- High sugar diets: Diets rich in sugars and refined carbohydrates can fuel Candida growth, as the fungus thrives on sugar.
How Is Vaginal Candidiasis Diagnosed?
A healthcare provider, typically a gynecologist, can diagnose vaginal candidiasis through:
- A physical examination of the affected area.
- A microscopic analysis of vaginal discharge to identify the presence of Candida.
- In recurrent or severe cases, additional tests may be conducted to rule out other conditions or identify less common Candida species.
Effective Treatment Options
Treatment for vaginal candidiasis is straightforward and varies depending on the severity of the infection. Common approaches include:
- Antifungal Medications:
- Topical treatments: Creams, ointments, or suppositories containing clotrimazole, miconazole, or similar antifungals are applied directly to the vagina.
- Oral treatments: Fluconazole is a widely prescribed oral medication, often effective in just one or two doses.
- Lifestyle Adjustments:
- Avoid tight, synthetic clothing and opt for breathable fabrics like cotton.
- Keep the vaginal area clean and dry, especially after exercise or swimming.
- Reduce sugar and carbohydrate intake to limit fungal growth.
- Home Remedies and Supportive Measures (consult a doctor before trying these):
- Probiotics: Lactobacillus supplements or yogurt with live cultures may help restore the natural balance of bacteria.
- Coconut oil: Known for its antifungal properties, it may offer relief when applied externally.
- Tea tree oil: Diluted tea tree oil can be used as a topical treatment, but it may irritate sensitive skin.
Preventing Vaginal Candidiasis
Prevention is often the best approach to avoid recurring infections. Simple strategies include:
- Maintain a balanced diet: Focus on whole foods, limit sugar, and include foods rich in probiotics, like yogurt and fermented vegetables.
- Practice proper hygiene: Use unscented soaps and avoid harsh chemicals or douches.
- Wear breathable clothing: Choose cotton underwear and avoid staying in wet clothing for extended periods.
- Manage stress: Chronic stress can weaken your immune system, making it harder for your body to fight off infections.
- Monitor medication use: If you need antibiotics, discuss with your doctor about preventive measures to protect your vaginal health.
When Should You Seek Medical Help?
Although vaginal candidiasis is common and treatable, certain situations require prompt medical attention:
- Recurrent infections (more than four times a year).
- Symptoms that persist despite treatment.
- Pregnancy, as infections can pose risks if not properly managed.
- Symptoms accompanied by fever, foul-smelling discharge, or severe pelvic pain (these could indicate other serious infections).
Additional Insights: Understanding Recurrent Candidiasis
For women experiencing frequent episodes of vaginal candidiasis, it’s crucial to explore underlying factors such as:
- Chronic illnesses or hormonal imbalances.
- Unaddressed stress or sleep deprivation, which weakens immunity.
- The possibility of antifungal resistance due to frequent use of medications.
Conclusion
Vaginal candidiasis is a common yet manageable condition that responds well to proper treatment and preventive measures. By maintaining a balanced lifestyle, practicing good hygiene, and seeking medical guidance when needed, you can minimize the risk of infections and improve your overall vaginal health. If you suspect you have vaginal candidiasis or experience recurrent symptoms, consult a healthcare professional for personalized advice and treatment options.

Dr. Sarah Miller is widely recognized as an influential leader in the healthcare field, with a career marked by excellence, innovation, and dedication to improving human well-being. Combining exceptional academic knowledge, clinical experience, and a deep commitment to research, she has become a reference in her specialty.





whoah this blog is great i like reading your posts.
Stay up the good work! You understand, many
persons are looking round for this info, you can help them greatly.
I like what you guys are up too. This type of clever work and exposure!
Keep up the wonderful works guys I’ve added you guys to my blogroll.
I visit each day a few web pages and sites to read articles, but this weblog offers feature based posts.
Excellent blog you have got here.. It’s hard to find quality writing like yours
nowadays. I truly appreciate individuals like you! Take care!!
After I initially commented I appear to have clicked the -Notify me when new comments are added- checkbox and now each time a
comment is added I recieve 4 emails with the exact same comment.
There has to be a means you are able to remove me from that service?
Many thanks!
Hello everything is fine?
just click on the email you received to unsubscribe
Hmm it looks like your blog ate my first comment (it was extremely long) so I guess I’ll just sum it up what I submitted and say,
I’m thoroughly enjoying your blog. I too am an aspiring blog writer but I’m still new to the whole thing.
Do you have any helpful hints for rookie blog writers?
I’d really appreciate it.
Oh my goodness! Amazing article dude! Thanks, However I am going
through issues with your RSS. I don’t understand why I can’t join it.
Is there anybody else having identical RSS issues? Anyone who knows the solution can you kindly respond?
Thanx!!
I’m not sure exactly why but this web site is loading incredibly slow for me.
Is anyone else having this problem or is it a issue on my end?
I’ll check back later on and see if the problem still
exists.
Good blog you’ve got here.. It’s hard to find high quality writing like yours these days.
I seriously appreciate individuals like you! Take care!!
Thank you to the whole team for your affection and above all for your time
We live in such a rush that we don’t even stop to contemplate a great text, good music, good company
The fact that you reserve some of this precious asset to read our material makes us extremely happy.
always come back
This site was… how do I say it? Relevant!! Finally I’ve
found something which helped me. Thank you!
Your mode of explaining everything in this post
is truly fastidious, all can effortlessly know it, Thanks a lot.
My family members always say that I am wasting my time here at web, except I know I am getting know-how all the time by reading such pleasant articles.
Pretty! This has been a really wonderful post.
Thanks for providing this information.
Welcome, the whole team was happy to read this. Gratitude for your life and here in our relevant information space
Howdy! This post couldn’t be written any better!
Reading this post reminds me of my previous room mate!
He always kept chatting about this. I will forward this write-up to him.
Pretty sure he will have a good read. Many thanks for sharing!
Thank you for being here!
What did you think of our blog?
Hey! Would you mind if I share your blog with my facebook group?
There’s a lot of folks that I think would really appreciate your content.
Please let me know. Thank you
First of all, thank you very much for being here.
Without you, this small space for sharing ideas and thoughts would not make sense.
Yes, we can share it. It will help us bring more information to people.
If you wish, leave the group link here so we can visit and join.
Today, I went to the beach with my kids. I found a sea shell and gave
it to my 4 year old daughter and said “You can hear the ocean if you put this to your ear.” She put the shell to her ear and screamed.
There was a hermit crab inside and it pinched her ear. She never wants to go back!
LoL I know this is entirely off topic but I had to tell someone!
Ahhh, what a wonderful story — and poor little girl! 😄 Even though it was a scary moment for her, it’s these unique memories that end up becoming unforgettable stories that you’ll laugh (a lot!) about in the future. Thank you for sharing something so personal and spontaneous here, that’s more important than it seems: it creates a real connection between us. This space isn’t just about content, but about people, experiences and those little everyday adventures that bring us closer. So, even though it’s off topic, know that I loved reading this — and you’re always more than welcome to share anything here!
After going over a number of the blog posts on your web page,
I really appreciate your way of blogging. I saved as a
favorite it to my bookmark website list and will be checking back in the near
future. Take a look at my website as well and let me know how
you feel.
Thank you so much! I’m so glad you enjoyed the style of the posts on the blog. Each text is carefully crafted to be informative, engaging, and easy to follow — so knowing that it’s working for you is great. If you have any topics you’d like to see explored here or want to share what you like most about the posts, I’m totally open to suggestions!